Home > Blog
BLOG

Prepare for the RMSK or RMSKS Exam
Get ready for the RMSK or RMSKS exam with key tips and prerequisites to achieve certification and advance your career in musculoskeletal imaging. ...more
Why MSK Ultrasound
November 05, 2024•2 min read

MSK Masters launches new website and learning platform
We've been anticipating and looking forward to this day for months, and are excited to release our new website and learning platform to all of our amazing customers (and visitors)! The website was com... ...more
Why MSK Ultrasound
September 15, 2023•2 min read

4 Valuable Ways MSK Ultrasound Could Benefit Your Practice or Career
Worldwide, more healthcare professionals are utilizing MSK ultrasound for examining conditions within joints, bones, and muscles. MSK (musculoskeletal) sonography enables medical practitioners to dia... ...more
Why MSK Ultrasound
September 01, 2023•5 min read

Adequate Training
Good morning, ladies and gentleman! This is your captain speaking. We want to thank you for flying with us today. On behalf of myself and the co-captain, we want to take a moment to let you know that ... ...more
Why MSK Ultrasound
August 02, 2023•1 min read
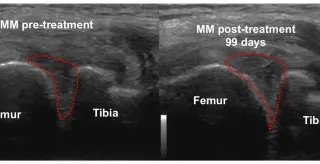
Serial Studies: A Picture is worth 1000 words
In my 5 years of training doctors involved in the orthopedic applications of bio-cellular/regenerative medicine therapies utilizing musculoskeletal ultrasound, I have received comments relative to imp... ...more
Why MSK Ultrasound
July 02, 2023•1 min read
MSK Masters Ultrasound diagnosis and guidance offers...
Discover how ultrasound diagnosis and guidance empower physicians to enhance outcomes in regenerative medicine, ensuring precise treatment and improved patient care. ...more
Why MSK Ultrasound
May 15, 2023•1 min read